In my journey through the intricacies of wound care, I've come to grasp the pivotal role that dressings play in healing. Not just any dressing will do—the careful selection between occlusive versus non-occlusive options is a critical decision for anyone looking to support recovery. With an eye on the differences between occlusive vs. non-occlusive dressings, I intend to navigate you through the maze of choices to identify suitable healing dressings for every type of wound. It's about matching the dressing to the wound's breathability needs and the body's natural repair processes.
Understanding the Basics of Wound Dressings
When I think about the myriad challenges posed in wound care, I'm keenly aware of the critical role wound dressings play in the healing process. It's fascinating how these medical materials serve dual purposes — they protect the wound from harmful bacteria and other external contaminants, while also creating an environment conducive to healing. Let's delve deeper into the purpose they serve and the various types available to those in need of wound care.
What Are Wound Dressings and Their Purpose?
At first glance, one might assume that a wound dressing simply covers a wound, but my experience in healthcare tells a broader story. The purpose of wound dressings is profound; they manage the wound environment to expedite healing, maintain optimal moisture levels, absorb exudate, and minimize patient discomfort. In addition, a well-selected dressing can also foster an optimal balance of moisture — not too wet, not too dry — assisting the body's natural reparative processes and protecting against infection.
Different Types of Dressings and Indications for Use
The selection of a dressing is highly dependent on the wound's characteristics and the healing stage. With indications for dressing use so varied, clinicians are fortunate to have an extensive array of types of wound dressings at their disposal.
For instance, hydrogel dressings for pressure ulcers are an excellent option for maintaining moisture in dry wounds, thus facilitating autolytic debridement and promoting healing. Understanding the types of hydrogel dressings is crucial for clinicians to tailor wound care to each patient's needs effectively.
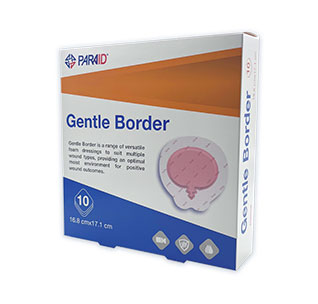
Additionally, silicone gel wound dressings offer a gentle yet effective option for managing scars and sensitive wounds, minimizing the risk of further trauma upon removal. For wounds with higher exudate, types of foam dressings for wounds provide excellent absorption, thereby reducing the risk of maceration and promoting a healthy healing environment.
Below is a table that breaks down different dressing types alongside their common indications, helping to delineate which may be more appropriate for a given wound scenario.
| Dressing Type | Characteristics | Common Indications | Examples |
|---|
| Adhesive | Easy to apply, absorbent, provides securement | Minor abrasions, post-surgical incisions | Band-Aid, Mepore |
| Alginate | Highly absorbent, derived from seaweed | Exudative wounds, burns, pressure ulcers | Kaltostat, AlgiSite |
| Foam | Moisture-retaining, cushioning | Moderate to highly exuding wounds, pressure ulcers | Mepilex, Allevyn |
| Hydrocolloid | Occlusive, form a gel with wound exudate | Dry to moderately exuding wounds, burns, pressure sores | DuoDERM, Comfeel |
| Hydrogel | Moisture donator, soothing | Dry, necrotic wounds, minor burns | Intrasite Gel, Solosite |
| Film dressing | Transparent, permeable to moisture vapor and oxygen | Secondary dressing, autolytic debridement of wounds | Tegaderm, Opsite |
Considering the types of wound dressings mentioned above, it’s evident that each has its own unique features that cater to different indications for dressing use. Deciding the perfect match requires a thoughtful examination of the wound's status, the ambient environment, and the patient's overall state of health. As we move forward, grasp this foundational knowledge as an integral component of effective wound management.
Occlusive vs. Non-occlusive Dressings: Core Differences
In my journey to understand wound care more deeply, I've found the differences between occlusive and non-occlusive dressings to be particularly significant. These two types of dressings can influence healing outcomes in distinct ways, and knowing when to use one over the other is a key part of effective wound management.
The Meaning of Occlusive Dressing
Occlusive dressings are fascinating in their function. By creating a hermetic seal over a wound, they prevent air and moisture from reaching the injured tissue. This meaning of occlusive dressing translates to a higher level of protection and moisture retention, which can be crucial for wounds that benefit from a moist healing environment.
Characteristics of Non-occlusive Bandages
On the other hand, the characteristics of non-occlusive bandages include their permeability to air and moisture. This trait allows for oxygen exchange and, depending on the material, a controlled evaporation of excess moisture. Non-occlusive dressings are less restrictive and can be a better choice for wounds requiring a drier environment to heal effectively.
Selecting the Right Type for Your Needs
Selecting suitable dressings is paramount, and I often consider several factors to make this decision. Factors like the wound's size, depth, exudate amount, and infection status all play crucial roles. With so many variables, it's important to have a solid understanding of the types of dressings available.
| Occlusive Dressings | Non-Occlusive Bandages |
|---|
| Air and moisture barrier | Permeable to air/moisture |
| Promote moist environment | Facilitate dry environment |
| Used for deeper, more severe wounds | Often used for superficial wounds or at the final healing stages |
| Reduce risk of infection by sealing off wound | Allow for better monitoring of the wound site |
| Can help in autolytic debridement | Supports natural drying & debridement |
Benefits of Using Occlusive Dressings
In my ongoing exploration of wound care, I've come to find occlusive dressings to be a cornerstone of effective treatment strategies, particularly for chronic or more troublesome wounds. They stand out for their ability to maintain a moist healing environment, a detail that has not escaped the notice of healthcare professionals. It's this humidity that keeps the wound bed adequately moist, thus averting the dreaded dry-out that can frankly impede the healing trajectory.
Let's talk about the core benefits of occlusive dressings. Firstly, these dressings are like a nurturing cocoon for the wound, fostering an enhanced healing process that could be a game-changer for patients. This process stems from the dressing's ability to prevent water vapor loss, keeping the cells well-hydrated and in a prime state for regeneration.
Healing in a moist environment helps to decrease the formation of scabs, which can facilitate a swifter and more cosmetically appealing healing process.
The occlusive nature means fewer dressing changes, leading to not only less disruption for the patient but also a potential reduction in care-related costs.
By sealing the wound, there's less chance of external contaminants complicating things, thereby lowering the risk of infection.
What truly makes these dressings exceptional, in my experience, is their versatility across a spectrum of wounds—from minor abrasions to severe burns. It's been my observation that the physiological benefits of maintaining a moist environment expedite the healing of such injuries. As I've delved into wound care options, occlusive dressings like hydrocolloid and hydrogel dressings consistently stand out. They're not the one-trick ponies of the dressing world; rather, they're multitasking maestros — protecting, nurturing, and optimizing wound recovery all at once.
When to Use Non-Occlusive Dressings Over Occlusive Ones
In the world of wound care, there’s a clear place and purpose for every type of dressing. While occlusive dressings play a pivotal role in maintaining moist healing environments, certain wounds benefit from a lighter touch—afforded by semi occlusive bandages. Let's delve into the instances that call for a breathable treatment option and how these bandages offer distinct wound healing advantages.
Advantages of Semi-Occlusive Bandages for Wound Healing
Semi-occlusive bandages, unlike their fully occlusive counterparts, strike a harmonious balance between protecting the wound and allowing vital air flow. This can be particularly beneficial during the latter stages of healing where the wound isn't at a high risk of infection and requires less intensive moisture retention. The advantage of facilitating natural drying and epithelialization—without completely forsaking moisture—makes semi occlusive bandages a compelling choice for clinicians and patients alike.
Scenarios Where Non-occlusive Dressings Are Preferred
While occlusive bandages are often recommended for heavily exudating wounds or those needing high-level protection from contaminants, there are several scenarios for non-occlusive dressings to shine. I’ve put together a table to illustrate the specific situations where non-occlusive dressings are the preferred route for better healing outcomes.
| Scenario | Advantages of Non-Occlusive Dressings |
|---|
| Post-operative wounds with low exudate | Lowers the risk of maceration while supporting sufficient moisture for healing |
| Minor abrasions and lacerations | Facilitates air exposure that is conducive for efficient tissue repair and regeneration |
| Acute wounds entering the late healing stages | Supports the transition from granulation to epithelialization process without overhydration |
| Chronic wounds with controlled exudate | Allows for necessary moisture retention while preventing the buildup of excessive moisture that can delay healing |
| Dry or minimally weeping wounds | Prevents desiccation of the wound bed with just enough moisture while allowing essential air contact |
Understanding when to opt for semi-occlusive bandages not only demonstrates a comprehensive knowledge in wound care but also ensures the patient's wound has the optimal conditions it needs to follow the natural healing trajectory. With the sophisticated variety of bandages available, utilizing non-occlusive options at the appropriate time can lead to expedited recovery and superior healing outcomes.
Exploring Semi-Occlusive and Sterile Occlusive Dressing Options
As we dive deeper into the world of wound care, the versatility of semi-occlusive dressings comes to the forefront, bridging the gap between full occlusion and complete exposure. Their intelligent design allows for a controlled healing environment suitable for a myriad of medical scenarios. And when it comes to fending off pathogens, the importance of sterile occlusive dressings cannot be overstated. They are the unsung heroes in the prevention of infection, safeguarding the wound with an impenetrable barrier.
Understanding Semi-Occlusive Dressings and Their Uses
I've observed firsthand that semi-occlusive dressings usage extends to cases ranging from simple day-to-day injuries to post-operative recovery. These dressings, characterized by their permeable nature, offer a partially moist healing environment, ideal for wounds that are not heavily exudating yet need protection from external contaminants.
Importance of Sterility in Occlusive Dressings
When a wound is at risk for infection, a sterile occlusive dressing is critical. Its aseptic barrier is key in maintaining the wound's cleanliness, which in my experience, not only helps in speeding up the repair but also safeguards the patient’s well-being, significantly minimizing the potential for septic complications.
Popular Products and Brand Considerations
Renowned dressing products like DuoDERM and Tegaderm have emerged as top picks in the industry due to their reliable performances in clinical settings. Quizzing colleagues and combing through caseloads, I've noticed a trend toward these popular dressing products when choosing optimal wound care supplies. Here’s a comparison of some leading brands and products:
| Product Name | Type | Indicated Use | Key Feature |
|---|
| DuoDERM | Hydrocolloid | Pressure Ulcers, Leg Ulcers | Conforms to body contours |
| Tegaderm | Transparent Film | I.V. Sites, Simple Wounds | Waterproof, Breathable |
| Mepitel | Semi-Occlusive | Skin Tears, Abrasions | Silicone adhesive, Minimizes trauma |
Whether you’re a healthcare professional or a caregiver, delving into the substantive properties of semi occlusive and sterile occlusive dressings, along with acknowledging their fundamental roles in modern medicine, cultivates a more informed approach to wound management.
Best Practices: How to Apply Moist to Dry and Wet to Dry Bandages
My experience in wound care has taught me that the tried-and-true methods of applying moist to dry dressing practices are about more than just covering a wound. These techniques serve as a gentle yet effective means of debridement, meticulously balancing the wound's natural moisture while fostering an environment conducive to healing. When it's time to apply a moist to dry dressing, I start by thoroughly cleaning the wound and surrounding skin to ward off infection and promote the best possible results.
The wet to dry bandage application process, in particular, deserves a diligent approach. I ensure the dressing is properly moistened – not drenched – to avoid maceration of healthy skin and place it on the wound carefully. This nuanced technique maintains the moisture level just right; the dressing will adhere to the dead tissue, which will be removed when the bandage is changed, without causing trauma to the wound bed. As I proceed, checking for any signs of irritation gives me the feedback needed to adjust the technique for subsequent changes.
Indeed, understanding and mastering these dressing applications are fundamental for anyone who cares for wounds, whether in a professional medical setting or at home. Each step I take is guided by the principle of promoting the best healing environment possible. My meticulous attention to the applying moist to dry dressing practices and the nuances of the wet to dry bandage application demonstrates that while these methods may be rooted in tradition, they are still relevant and effective in contemporary wound management scenarios.
 English
English